-

When it comes to natural supplements, few are as intriguing — or as easy to mix up — as colostrum and colostrinin. While they both come from the same source (early mammalian milk), they serve very different roles in health and wellness. Let’s break it down clearly, and then zoom in on the most exciting…
-

If you’ve ever felt burning, tingling, numbness, or stabbing sensations in your hands or feet, you may have wondered: Is this neuropathy or just nerve pain? Are they the same thing? It’s a common question—and an important one. While people often use the terms interchangeably, neuropathy and nerve pain are not identical. Understanding the difference…
-

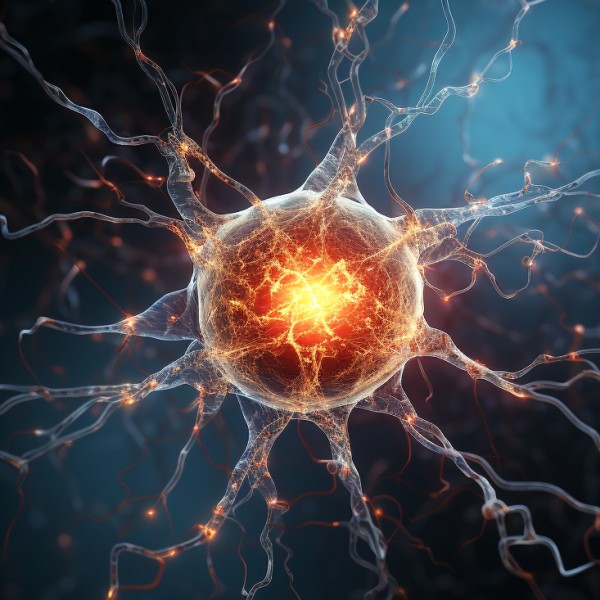
Neuropathy, a condition characterized by nerve damage, can manifest in various ways, including numbness, pain, and weakness in the hands and feet. The causes of neuropathy are numerous and include diabetes, chemotherapy, autoimmune diseases, and even infections. While traditional treatments focus on alleviating symptoms, researchers are continually exploring new therapies to address the root causes…
-

Finding Real Relief:How Acupuncture’s Ancient Wisdom Meets Modern Science for Neuropathy Neuropathy, a complex condition marked by disruptive pain, numbness, and a host of uncomfortable sensations, casts a long shadow on the daily lives of many. While conventional treatments offer relief for some, others understandably seek alternative paths. Enter acupuncture, an age-old practice from the…